Understanding Sperm Health: Count, Motility, and Morphology
When it comes to fertility, the conversation often centers around ovulation, egg quality, and the female reproductive system. But here’s the truth—sperm health plays an equally important role in conception. It takes two to make a baby, after all.
Whether you’re actively trying to conceive or just planning for the future, understanding the basics of sperm health—especially sperm count, motility, and morphology—can empower you with the knowledge to make informed choices. Don’t worry, we’ll break it all down without diving into overwhelming medical jargon.
Let’s have an open, real talk about what sperm are, what makes them healthy, and how to support that health naturally and intentionally.
Why Sperm Health Matters?
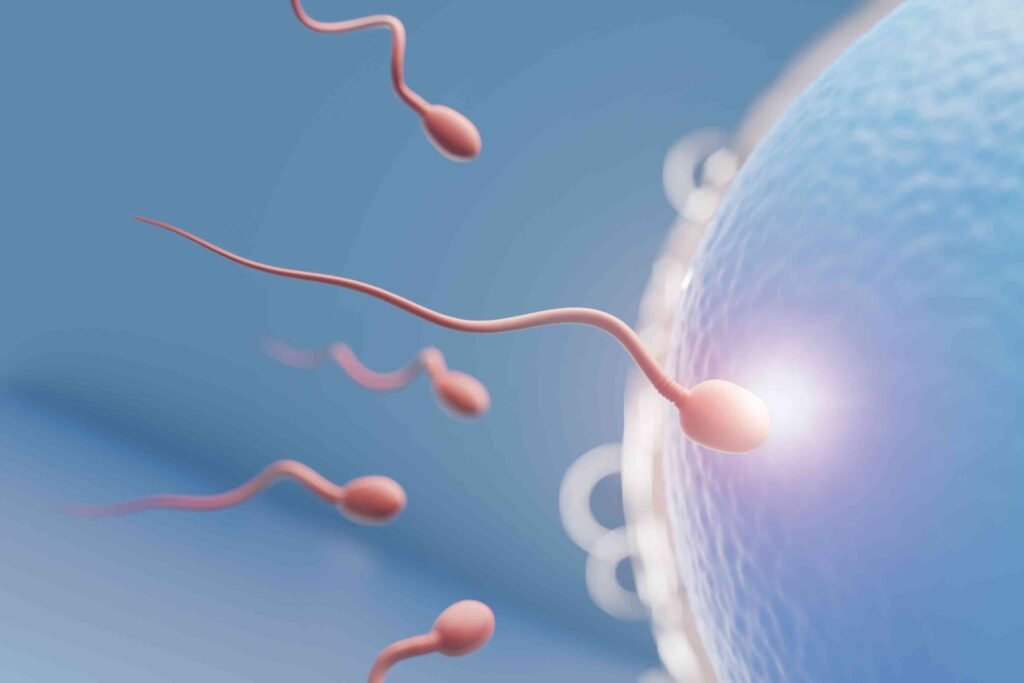
Before we get into the nitty-gritty, let’s take a moment to appreciate just how fascinating sperm really are. Each ejaculate contains millions of tiny swimmers, and just one of them has the job of fertilizing an egg. That’s a lot of competition for such a tiny cell.
But not all sperm are created equal. Some swim faster, some have better structure, and some might not function well at all. This is where the concept of sperm health becomes crucial. Poor sperm quality can make it harder to conceive, even if the female partner is perfectly fertile.
When we talk about sperm health, we’re mainly looking at three key factors:
a. Count – how many sperm are present
b. Motility – how well they swim
c. Morphology – how normal they look in shape and structure
Sperm Count: Strength in Numbers
What Is Sperm Count?
Sperm count refers to the number of sperm present in a given amount of semen. According to the World Health Organization (WHO), a normal sperm count is at least 15 million sperm per milliliter of semen. Anything below that may be considered low (a condition called oligospermia).
Why Does It Matters?
The more sperm you have, the better your chances of one successfully reaching and fertilizing the egg. Low sperm count doesn’t mean pregnancy is impossible—it just means the odds are a little slimmer and might take longer or require assistance.

Factors That Affect Sperm Count
a. Heat: Testicles function best at slightly cooler temperatures. Prolonged exposure to heat (like hot tubs or tight underwear) can temporarily reduce sperm count.
b. Toxins: Exposure to chemicals, pesticides, and heavy metals can negatively impact sperm production.
c. Substance use: Smoking, excessive alcohol, and drug use (including anabolic steroids) are known sperm killers.
d. Health issues: Conditions like varicocele (enlarged veins in the scrotum) or hormonal imbalances can impair sperm production.
What You Can Do?
If you’re looking to optimize your sperm count, the first step is often lifestyle-related. Wearing looser underwear, quitting smoking, and maintaining a healthy weight are all great starting points. We’ll get into more specific action steps a little later in the blog.
Sperm Motility: The Power to Swim
What Is Sperm Motility?
Motility is just a fancy word for movement. Sperm motility refers to how well the sperm can move through the female reproductive tract to reach the egg. There are two types: progressive (straight-line or purposeful movement) and non-progressive (wiggling in place or moving erratically).
Good motility means sperm are active and swimming in the right direction—key to actually reaching the egg. According to WHO, 40% motility is considered the lower limit of what’s normal, with 32% or more being progressively motile.
Why Does It Matters?
Even if you have a high sperm count, poor motility can still make conception difficult. Sperms need to travel a pretty long distance (in microscopic terms), and if they aren’t moving effectively, they won’t make it.
Causes of Poor Motility
a. Oxidative stress: High levels of free radicals in the body can damage sperm cells and affect how they move.
b. Lifestyle choices: Poor diet, lack of exercise, and exposure to environmental toxins can all impact motility.
c. Age: While men can remain fertile longer than women, sperm motility does decline with age, especially after 40.
Improving Motility
Antioxidants like vitamin C, vitamin E, and CoQ10 have been shown to support better sperm motility. Reducing inflammation in the body through diet and exercise is another powerful way to give your sperm a mobility boost.

Sperm Morphology: Form Meets Function
What Is Morphology?
Morphology refers to the size and shape of sperm. Under a microscope, a healthy sperm has an oval head and a long tail—ideal for swimming and penetrating the egg. Abnormally shaped sperm (like those with double heads, short tails, or bent necks) may not function properly.
In a standard semen analysis, morphology is graded based on the percentage of sperm that look normal. Typically, anything above 4% normal forms is considered within the normal range.
Why It Matters?
Sperm with abnormal morphology may struggle to reach or fertilize an egg. That said, morphology tends to be the trickiest of the three factors—many men with low morphology percentages still go on to conceive naturally. It’s a piece of the puzzle, not the whole picture.
Causes of Poor Morphology
a. Infections: STIs or unresolved infections in the reproductive tract can lead to malformed sperm.
b. Toxins: Exposure to plasticizers, radiation, and pollution can affect sperm development.
c. Genetics: Sometimes, morphology issues are simply inherited and not something easily changed.
Lifestyle Tips to Support Sperm Health
So what can you actually do to improve or protect your sperm quality? Fortunately, there are several manageable changes that can make a big difference in supporting overall sperm health:
1. Eat a Fertility-Friendly Diet
Foods rich in antioxidants, omega-3 fatty acids, zinc, selenium, and folate are great for sperm. Think leafy greens, berries, fatty fish, nuts, and seeds.
Avoid trans fats, processed meats, and sugary foods—they’ve been linked to reduced sperm quality.

2. Stay Active (But Don’t Overdo It)
Moderate exercise boosts circulation, regulates hormones, and supports sperm production. But excessive endurance training or steroid use can backfire. Balance is key.
3. Keep Things Cool
Avoid prolonged exposure to heat: hot tubs, saunas, laptops on your lap, or anything else that could raise testicular temperature. Even switching to boxers over briefs can help.
4. Cut the Toxins
a. Quit smoking
b. Limit alcohol
c. Stay away from recreational drugs
d. Reduce exposure to pesticides, plastics (like BPA), and harsh cleaning products
These toxins can reduce sperm count and mess with hormone levels.
5. Manage Stress
Chronic stress affects everything from testosterone production to sexual performance. Meditation, therapy, journaling, or even just daily walks can help lower cortisol and support sperm health.
6. Get Regular Checkups
If you’re thinking about starting a family, get a semen analysis done. It’s painless, affordable, and offers a ton of insight. If there are any red flags, it’s better to know early so you can address them.
When to See a Fertility Specialist?
If you and your partner have been trying to conceive for a year or six months if the female partner is over 35), it may be time to check in with a fertility specialist.
A basic semen analysis can assess sperm count, motility, and morphology, and additional testing can reveal any underlying issues like hormone imbalances, infections, or genetic concerns.
The good news? Many sperm health problems are treatable. From simple lifestyle tweaks to medical interventions, there are a variety of options to help boost fertility.

Debunking Common Myths About Sperm Health
Let’s bust a few myths that still make the rounds.
Myth 1: “If I can ejaculate, my sperm must be fine.”
Not quite. Semen and sperm are not the same thing. You can ejaculate a normal-looking amount of semen and still have a low sperm count or poor motility.
Myth 2: “Age doesn’t matter for men.”
While men remain fertile longer than women, sperm health does decline with age. Quality tends to start dipping after age 40, with increased risks of miscarriage or genetic issues.
Myth 3: “Tight underwear is the main cause of infertility.”
It’s not the only factor, but it’s true that heat plays a role. If you’re trying to optimize sperm production, consider switching to looser-fitting underwear and avoiding prolonged heat exposure.
The Emotional Side of Male Fertility
Talking about sperm health isn’t always easy. There’s still a stigma around male fertility, and many men feel uncomfortable or even ashamed if something isn’t working as expected.
But here’s the truth: Male infertility is more common than people think, and it doesn’t define your masculinity, worth, or potential as a father.
It takes strength to talk about these things and even more strength to take action. If something feels off or you’re having trouble conceiving, speak up. You’re not alone, and support is out there.
Final Thoughts:
Sperm health is a major factor in fertility, and the good news is—it’s often something you can improve. Understanding your sperm count, motility, and morphology gives you valuable insight, whether you’re trying to conceive now or just thinking about the future.
Being proactive doesn’t mean something’s wrong—it means you care. And taking steps to support your reproductive health now could make all the difference later.
Whether you’re at the start of your fertility journey or somewhere in the middle, remember this: knowledge is power, and your body is capable of incredible things—even the tiniest cells have potential.