If you’ve ever experienced heartburn or that uncomfortable burning sensation in your chest after a meal, you might already be familiar with Gastroesophageal Reflux Disease (GERD), even if you didn’t know it by name. GERD is a common digestive disorder, but despite its prevalence, many people don’t fully understand what it is, why it happens, or how it can impact their daily lives. Let’s take a closer look at GERD, its causes, and why understanding it is the first step toward relief.
What is Gastroesophageal Reflux Disease?
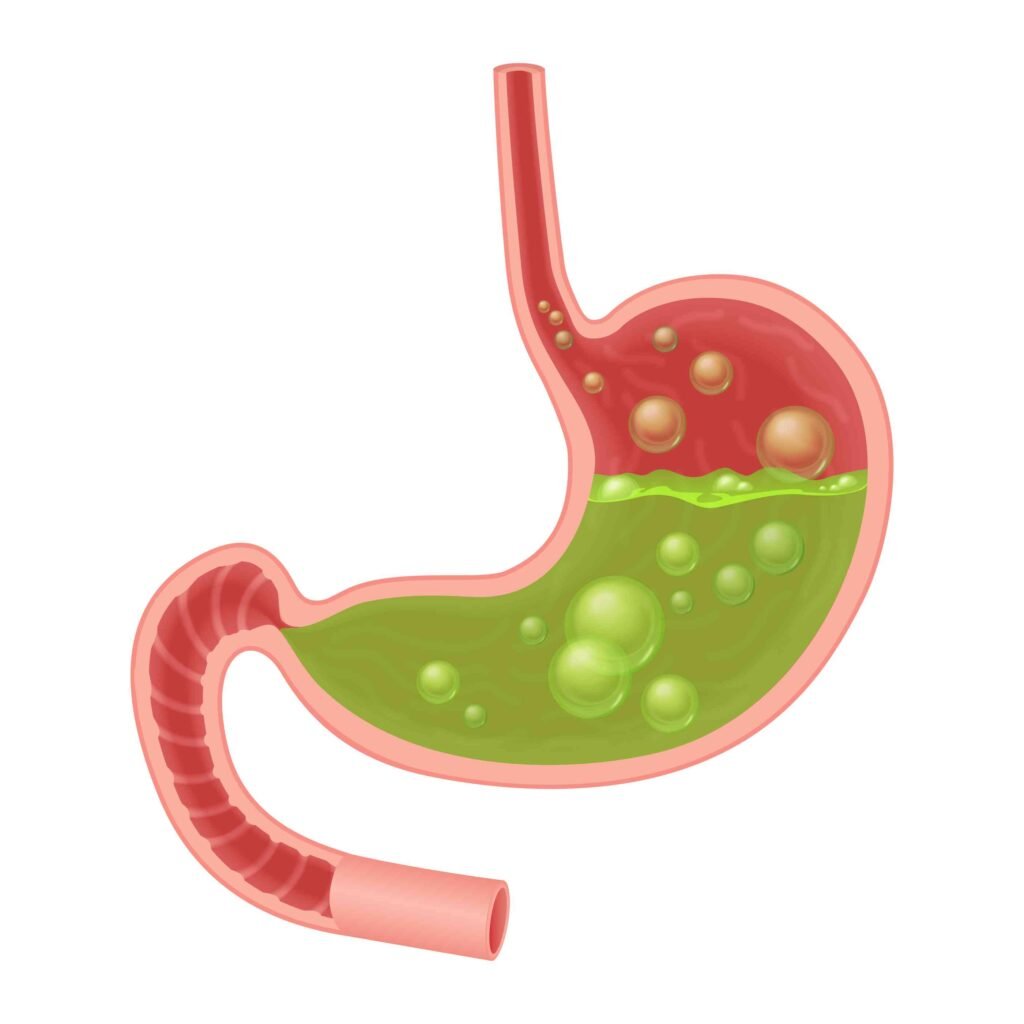
At its core, Gastroesophageal Reflux Disease is a condition where stomach acid flows back (or “refluxes”) into the esophagus, the tube that connects your mouth to your stomach. This happens because the lower esophageal sphincter (LES)—a ring of muscle at the end of your esophagus—fails to close properly or relaxes too often. When this occurs, stomach acid can irritate the esophagus lining, leading to symptoms like heartburn, regurgitation, and even chest pain.
While occasional acid reflux is normal and happens to many people, GERD is diagnosed when reflux happens frequently—usually more than twice a week—and starts to interfere with your daily life.

Common Symptoms of Gastroesophageal Reflux Disease
The symptoms of GERD can vary from person to person, but some are more common than others. These include:
- Heartburn: A burning sensation in the chest, often after eating or when lying down.
- Regurgitation: The sensation of stomach contents (including acid) coming back up into the throat or mouth.
- Chest Pain: Sometimes GERD can cause discomfort that feels like a tightness or burning in the chest.
- Difficulty Swallowing: Known as dysphagia, this symptom can occur due to inflammation or narrowing of the esophagus.
- Chronic Cough or Hoarseness: Acid reflux can irritate the throat and vocal cords, leading to persistent coughing or voice changes.

It’s worth noting that not everyone with GERD experiences heartburn. Some people, especially older adults, may have atypical symptoms like unexplained nausea, bad breath, or even dental erosion caused by stomach acid.
What Causes Gastroesophageal Reflux Disease?
To better understand Gastroesophageal Reflux Disease, we need to dive into the factors that cause it. GERD is rarely caused by one issue alone; instead, it’s often the result of a combination of factors. These can include:
1. Weakness or Dysfunction of the Lower Esophageal Sphincter (LES)
The LES acts as a barrier between your stomach and esophagus, preventing stomach contents from flowing back upward. When the LES weakens or becomes too relaxed, it can’t do its job effectively, allowing acid to escape. This malfunction is one of the leading causes of GERD.
2. Diet and Eating Habits
Certain foods and beverages can trigger or worsen GERD symptoms. Some common culprits include:
- Fatty or fried foods
- Spicy dishes
- Citrus fruits
- Chocolate
- Caffeinated drinks like coffee and tea
- Alcohol
- Carbonated beverages
Eating large meals or lying down shortly after eating can also increase the risk of reflux, as these habits put extra pressure on the stomach.

3. Obesity
Excess weight, especially around the abdomen, increases pressure on the stomach. This can cause the LES to weaken and make reflux more likely. Studies have shown that losing even a small amount of weight can significantly reduce GERD symptoms.
4. Hiatal Hernia
A hiatal hernia occurs when part of the stomach pushes up through the diaphragm and into the chest cavity. This condition can disrupt the normal functioning of the LES and contribute to GERD.
5. Smoking
Smoking is a known risk factor for GERD. It weakens the LES, reduces saliva production (which helps neutralize acid), and can increase stomach acid production.
6. Pregnancy
Many women experience GERD symptoms during pregnancy, particularly in the second and third trimesters. Hormonal changes and the physical pressure of the growing uterus on the stomach can both contribute to reflux.
7. Medications
Certain medications, such as aspirin, ibuprofen, muscle relaxants, and blood pressure drugs, can relax the LES or irritate the esophagus, leading to GERD symptoms.
How Does Lifestyle Impact GERD?
While factors like obesity, pregnancy, and certain medical conditions can make someone more susceptible to GERD, lifestyle habits play a significant role in both the development and management of the condition.
- Eating Late at Night: Lying down after a meal makes it easier for stomach acid to flow back into the esophagus. Try to finish eating at least 2-3 hours before bedtime.

- Wearing Tight Clothing: Clothing that puts pressure on the abdomen (like belts or tight jeans) can worsen reflux symptoms.
- Inadequate Exercise: While heavy exercise after a meal may trigger reflux, regular moderate exercise can help manage weight and improve digestion.
- Stress: High stress levels don’t directly cause GERD, but they can worsen symptoms by increasing stomach acid production or leading to unhealthy eating habits.
Diagnosing Gastroesophageal Reflux Disease
If you suspect you have GERD, it’s important to consult a doctor. Diagnosis often involves:
- Medical History Review: Your doctor will ask about your symptoms, eating habits, and any medications you’re taking.
- Endoscopy: This procedure involves inserting a thin, flexible tube with a camera into your esophagus to check for inflammation or damage.

- pH Monitoring: A small device is placed in your esophagus to measure how often stomach acid enters and how long it stays there.
- Manometry: This test measures the strength and coordination of your esophageal muscles, including the LES.
Complications of Untreated GERD
Ignoring Gastroesophageal Reflux Disease can lead to more serious health problems over time, including:
- Esophagitis: Inflammation of the esophagus due to repeated acid exposure.
- Esophageal Stricture: Narrowing of the esophagus, making swallowing difficult.
- Barrett’s Esophagus: A condition where the esophageal lining changes, increasing the risk of esophageal cancer.
- Dental Issues: Chronic acid exposure can erode tooth enamel.
Managing and Treating Gastroesophageal Reflux Disease
The good news is that GERD can often be managed with a combination of lifestyle changes, medications, and in some cases, medical procedures.
Lifestyle Modifications
- Eat Smaller Meals: This reduces pressure on the LES and stomach.
- Avoid Trigger Foods: Keep a food diary to identify and eliminate foods that worsen symptoms.
- Elevate the Head of Your Bed: Sleeping with your upper body elevated can prevent acid reflux at night.
- Quit Smoking: This can improve LES function and overall digestive health.

Medications
- Antacids: Provide quick relief by neutralizing stomach acid.
- H2 Receptor Blockers: Reduce acid production in the stomach.
- Proton Pump Inhibitors (PPIs): Block acid production and allow the esophagus to heal.
Medical Procedures
- Fundoplication: A surgical procedure where the upper part of the stomach is wrapped around the LES to strengthen it.
- LINX Device: A ring of magnetic beads is placed around the LES to prevent reflux.
Conclusion
While Gastroesophageal Reflux Disease can be uncomfortable and disruptive, it’s a manageable condition with the right approach. Understanding your triggers, making lifestyle changes, and seeking medical help when needed can significantly improve your quality of life. Remember, small adjustments can make a big difference in keeping GERD under control.
If you’re experiencing persistent reflux symptoms, don’t wait—reach out to a healthcare professional and take the first step toward relief and better digestive health. After all, no one deserves to live with the discomfort of GERD when solutions are within reach.