The Role of Embryo Quality in IVF Success Rates
In the intricate journey of in vitro fertilization (IVF), the importance of every step cannot be overstated. Among the many factors influencing the success of IVF, embryo quality stands out as a critical determinant. The health and viability of embryos are central to achieving a successful pregnancy. This blog explores the pivotal role of embryo quality in IVF outcomes, the factors affecting it, and ways to optimize it.
What is Embryo Quality?
Embryo quality refers to the health, viability, and potential of an embryo to develop into a healthy pregnancy. During the IVF process, embryos are created by fertilizing eggs with sperm in a laboratory. These embryos are then carefully evaluated to determine their suitability for transfer into the uterus.
Embryologists use specific grading systems to assess embryo quality, considering characteristics such as cell division, symmetry, and the presence of fragmentation. High-quality embryos are more likely to implant successfully, leading to a healthy pregnancy.

Why Does Embryo Quality Matter in IVF?
The quality of embryos plays a decisive role in IVF success for several reasons:
1. Improved Implantation Rates
High-quality embryos have a greater chance of implanting in the uterine lining, increasing the likelihood of pregnancy. Their optimal structure supports better interaction with the endometrium.
2. Reduced Risk of Miscarriage
Embryos with chromosomal abnormalities or poor morphology are more prone to miscarriages. High-quality embryos, on the other hand, significantly lower this risk.

3. Efficient Treatment Cycles
Better quality of embryo can reduce the need for multiple IVF cycles, saving couples both time and emotional energy. It also minimizes the financial burden of repeated treatments.
How is Embryo Quality Assessed?
Embryo quality is typically evaluated in two stages of development:
1. Cleavage-Stage Embryos (Day 2 or 3)
- Graded based on the number of cells, symmetry, and the level of fragmentation.
- High-quality cleavage-stage embryos usually have 6-8 evenly sized cells and minimal fragmentation.
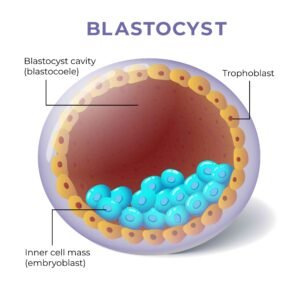
2. Blastocyst-Stage Embryos (Day 5 or 6)
- Assessed for the quality of the inner cell mass (which forms the fetus) and the trophectoderm (which forms the placenta).
- Blastocysts are considered optimal if they show proper expansion and well-defined structures.
While these evaluations provide valuable insights, the true potential of an embryo often depends on genetic health, which is why additional testing may be recommended.
Factors Influencing Embryo Quality
Embryo quality is influenced by various factors, including genetics, environment, and medical conditions. Let’s explore some key contributors:
1. Age
The age of the person providing the eggs is one of the most significant factors. Younger eggs typically have fewer chromosomal abnormalities, resulting in higher-quality embryos. Women over 35 may face challenges due to declining egg quality.
2. Sperm Health
The quality of sperm plays an equally vital role in embryo development. Factors like sperm motility, morphology, and DNA integrity affect fertilization and subsequent embryo quality.

3. Laboratory Conditions
The expertise of the embryology team and the quality of the IVF lab are critical. Advanced technology, precise handling, and controlled conditions significantly enhance embryo quality.
4. Lifestyle Choices
Smoking, excessive alcohol consumption, poor diet, and high stress levels can negatively impact both egg and sperm quality, reducing the chances of forming healthy embryos.
5. Underlying Medical Conditions
Conditions such as polycystic ovary syndrome (PCOS), endometriosis, or untreated infections can affect embryo quality. Proper diagnosis and management of these conditions are essential before undergoing IVF.
Can Poor-Quality Embryos Still Lead to Pregnancy?
It’s important to note that while high-quality embryos have the best chances of success, even embryos with less-than-optimal grades can sometimes result in successful pregnancies. Factors like uterine receptivity and the overall health of the person undergoing IVF also play crucial roles. Advanced techniques such as preimplantation genetic testing (PGT) can further help identify embryos with the best potential for success.
The Role of Genetic Testing in Embryo Quality
Preimplantation genetic testing (PGT) is a powerful tool used to assess the chromosomal health of embryos. Even visually perfect embryos may carry chromosomal abnormalities that could prevent implantation or result in miscarriage. PGT helps identify chromosomally normal (euploid) embryos, increasing the chances of a healthy pregnancy and live birth.
How to Improve Embryo Quality?
While some factors affecting the quality of embryo are beyond our control, others can be managed with conscious effort. Here are some practical tips to optimize embryo quality:
1. Adopt a Healthy Lifestyle
A balanced diet rich in antioxidants, vitamins, and omega-3 fatty acids can support egg and sperm health. Avoid smoking and excessive alcohol consumption, as these can negatively impact reproductive health.
2. Maintain a Healthy Weight
Being underweight or overweight can disrupt hormonal balance and fertility. Strive for a healthy BMI to create the best conditions for embryo development.
3. Reduce Stress
Chronic stress can interfere with hormone levels and reproductive function. Incorporating stress-reducing practices like meditation, yoga, or counseling can improve overall fertility.
4. Consider Supplements
Supplements like CoQ10, DHEA, and folic acid may improve egg and sperm quality. However, always consult your doctor before starting any supplements.

Conclusion:
Embryo quality is undeniably one of the most important factors in determining IVF success rates. From implantation to pregnancy outcomes, the health and viability of embryos shape the entire journey. Understanding the factors that influence quality of the embryo and taking steps to optimize it can significantly improve your chances of success.
While the science of IVF continues to advance, your determination and hope are equally vital. By working closely with a trusted fertility team and focusing on what you can control, you can navigate the path to parenthood with confidence. Remember, every journey is unique, and every step forward is a testament to your strength.


