Managing Chronic Pancreatitis with Surgical Interventions
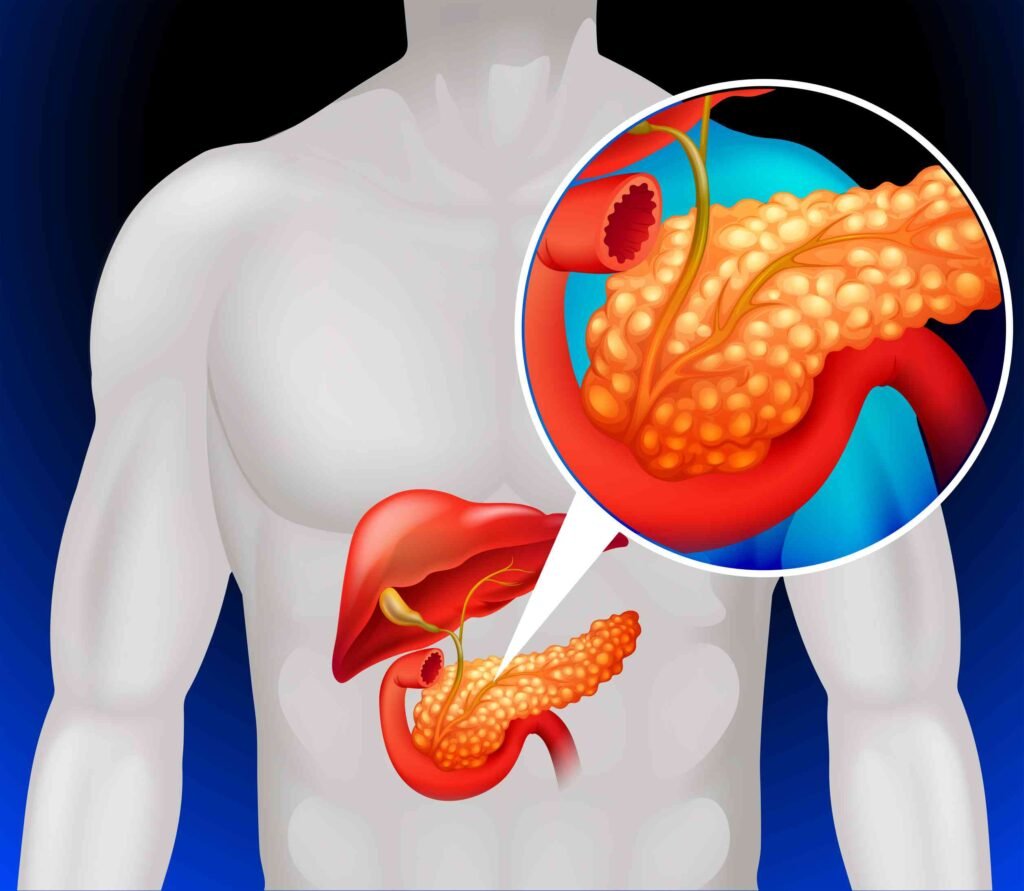
Chronic pancreatitis is a complex and often debilitating condition that affects the pancreas, an organ critical for digestion and blood sugar regulation. Living with this condition can be challenging, as it leads to persistent inflammation, scarring, and damage to the pancreas over time. While medical therapies, lifestyle changes, and pain management are often the first lines of treatment, some patients may require surgical intervention to alleviate symptoms and improve their quality of life.
In this blog, we’ll explore the role of surgical options in managing chronic pancreatitis, the scenarios in which surgery becomes necessary, and what patients can expect before, during, and after these procedures.
What is Chronic Pancreatitis?
To understand why surgical interventions might be needed, it’s essential to grasp what chronic pancreatitis entails. This condition occurs when the pancreas undergoes long-term inflammation, leading to irreversible damage. Unlike acute pancreatitis, which comes on suddenly and often resolves with treatment, chronic pancreatitis is a progressive disease. It can result in significant pain, malnutrition, and complications such as diabetes or pancreatic insufficiency.
Common causes include long-term alcohol abuse, genetic predispositions, autoimmune disorders, or even blockages in the pancreatic ducts. Regardless of the underlying cause, the persistent inflammation creates scar tissue that affects the pancreas’s ability to function properly.
When is Surgery Needed for Chronic Pancreatitis?
For many individuals with chronic pancreatitis, conservative treatments like enzyme replacement therapy, dietary modifications, and pain medications provide adequate symptom control. However, surgery may become necessary when:
- Pain Becomes Unmanageable: Severe abdominal pain that doesn’t respond to other treatments can significantly impact a person’s quality of life. Surgery may help by addressing the root cause of the pain.
- Complications Arise: Chronic pancreatitis can lead to complications such as bile duct obstructions, pancreatic pseudocysts, or even the development of pancreatic cancer. Surgery can help manage or prevent these issues.
- Pancreatic Function Deteriorates: When the pancreas can no longer produce sufficient digestive enzymes or insulin, surgical options may help preserve what remains of its function.

Surgical Options for Chronic Pancreatitis
1. Pancreatic Drainage Procedures
One of the primary goals of surgery in chronic pancreatitis is to relieve blockages in the pancreatic duct, which can contribute to pain and further damage. A common approach is lateral pancreaticojejunostomy, also known as the Puestow procedure. This involves creating a new pathway to allow pancreatic juices to flow more freely into the intestines, bypassing obstructions.
This type of surgery is often recommended for patients whose main pancreatic duct is significantly dilated due to blockages or scar tissue.
2. Resection Procedures
In some cases, parts of the pancreas may need to be removed if they are significantly damaged or if the pain is localized to a specific area. Common resection procedures include:
- Distal Pancreatectomy: Removes the tail of the pancreas, often in cases where cysts or tumors are present.
- Whipple Procedure (Pancreaticoduodenectomy): Removes the head of the pancreas along with part of the small intestine and bile duct. This is a more complex procedure often used when complications like cancer are suspected.
3. Total Pancreatectomy with Islet Autotransplantation (TPIAT)
This advanced surgical option involves removing the entire pancreas to eliminate pain and stop disease progression. Since the pancreas produces insulin, losing it would typically result in diabetes. However, TPIAT includes a process where the patient’s insulin-producing islet cells are transplanted into their liver, where they can continue to produce insulin.
This procedure is typically reserved for severe, refractory cases of chronic pancreatitis and offers hope to patients who have exhausted other treatment options.

4. Cyst or Pseudocyst Drainage
Pseudocysts, fluid-filled sacs that can develop in the pancreas due to chronic inflammation, may require surgical drainage if they become large, painful, or infected. This can often be done minimally invasively using endoscopic techniques.
Risks and Benefits of Surgery for Chronic Pancreatitis
Like any surgical procedure, interventions for chronic pancreatitis come with risks and benefits. Understanding these can help patients make informed decisions.
Benefits:
- Pain Relief: Many patients experience significant, if not complete, relief from chronic abdominal pain after surgery.
- Improved Quality of Life: Addressing complications and reducing symptoms can help patients return to daily activities.
- Prevention of Complications: Surgery can help prevent more severe issues, such as infections or cancer, that might arise from untreated chronic pancreatitis.
Risks:
- Surgical Complications: These may include bleeding, infection, or problems related to anesthesia.
- Diabetes: Removing part or all of the pancreas can lead to insulin dependence.
- Digestive Issues: Patients may require lifelong enzyme supplementation to aid digestion if significant portions of the pancreas are removed.

It’s crucial to work closely with a multidisciplinary team of healthcare providers to weigh these risks against potential benefits and decide on the most appropriate course of action.
Preparing for Surgery
If surgery becomes the recommended path for managing chronic pancreatitis, preparation is key to ensuring the best possible outcome. Your medical team will conduct a thorough evaluation, including imaging studies and blood tests, to determine the most suitable surgical approach.
Patients are typically advised to stop smoking, limit alcohol intake, and manage their nutrition before surgery to optimize their recovery. In some cases, preoperative interventions, such as endoscopic procedures, may be performed to alleviate immediate issues or improve surgical outcomes.
Recovery and Life After Surgery
Recovery times vary depending on the type of surgery performed. For minimally invasive procedures like pseudocyst drainage, recovery may take just a few weeks, while more extensive surgeries like a Whipple procedure or total pancreatectomy require longer healing times and intensive follow-up care.
What to Expect During Recovery:
- Pain Management: Pain is common in the weeks following surgery but can be controlled with medications and other supportive therapies.
- Dietary Changes: After surgery, many patients need to follow a modified diet and may require enzyme supplements to aid digestion.
- Ongoing Monitoring: Regular check-ups with your healthcare team will help ensure proper healing and monitor for any long-term complications.

While surgery can be life-changing, it’s not always a cure for chronic pancreatitis. Pain relief and improved quality of life are the primary goals, but some patients may still require ongoing treatment to manage symptoms and maintain pancreatic function.
The Emotional Toll of Chronic Pancreatitis and Surgery
Living with chronic pancreatitis can be emotionally draining, and the decision to undergo surgery is not taken lightly. It’s normal to feel a mix of hope and apprehension about the outcome. Connecting with support groups, counseling services, or others who have undergone similar procedures can provide valuable encouragement and insight.
Conclusion: Taking Charge of Chronic Pancreatitis
Managing chronic pancreatitis is a journey, and surgical interventions can be an important step for those who haven’t found relief through other treatments. While the idea of surgery may feel daunting, these procedures are often life-changing, offering significant pain relief and a path to a better quality of life.
If you or a loved one is struggling with chronic pancreatitis, talk openly with your healthcare provider about all available options, including surgical ones. Remember, you’re not alone in this fight, and there is hope for a brighter, healthier future.