The Role of Male Fertility in IVF
When it comes to infertility discussions, the focus often gravitates toward female reproductive health. However, male fertility plays an equally vital role in conception, especially in assisted reproductive technologies like IVF (In Vitro Fertilization). While it’s true that women undergo more rigorous physical processes in IVF, the male partner’s fertility directly impacts the chances of success. In this blog, we’ll explore why male fertility is important, the factors affecting it, and how it influences IVF outcomes.
Understanding Male Fertility in IVF
At its core, male fertility refers to the ability of a man to produce healthy sperm that can successfully fertilize an egg. This might sound straightforward, but achieving this “fertilization” isn’t always as simple as it seems. With male infertility contributing to nearly 40-50% of all infertility cases globally, it’s clear that this aspect deserves equal attention during the IVF process.
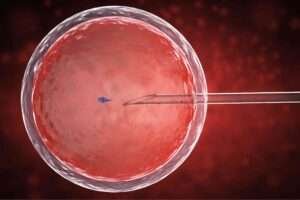
IVF is a complex procedure that involves retrieving eggs from the female partner, fertilizing them in a lab with sperm, and implanting the resulting embryo(s) into the woman’s uterus. For this process to be successful, the quality, quantity, and motility of sperm matter significantly.
If male fertility issues are detected, specialists may recommend additional procedures, such as ICSI (Intracytoplasmic Sperm Injection), where a single healthy sperm is injected directly into the egg to increase the chances of fertilization.
The bottom line? Healthy sperm is vital for IVF success, and male fertility is a significant factor in determining whether or not the process will result in pregnancy.
Causes of Male Fertility Issues in IVF
The reasons for reduced male fertility can range from lifestyle habits to medical conditions. Identifying these issues early helps doctors tailor the IVF process to the couple’s specific needs.
1. Sperm Quality and Quantity
One of the most critical factors affecting male fertility is sperm health. Sperm parameters are assessed based on:
- Concentration: The number of sperm per milliliter of semen.
- Motility: How effectively the sperm can swim toward the egg.
- Morphology: The shape and structure of the sperm, as abnormal forms can hinder fertilization.
Even if a man’s sperm count appears “normal,” issues like poor motility or abnormal morphology can still reduce the chances of success during IVF. Advanced semen analysis helps fertility specialists identify these concerns.

2. Hormonal Imbalances
Hormones play a major role in male fertility. Testosterone and other hormones regulate sperm production, and imbalances can lead to reduced sperm count or poor-quality sperm. Conditions like hypogonadism or thyroid disorders can directly impact sperm health.
3. Varicocele
A varicocele refers to enlarged veins in the scrotum, which can affect testicular function and lead to low sperm production. Varicoceles are one of the leading treatable causes of male infertility.
4. Lifestyle Factors
Diet, stress, smoking, alcohol consumption, and exposure to environmental toxins can all contribute to reduced male fertility. A sedentary lifestyle and obesity are also linked to poor sperm health, further complicating the IVF process.

5. Genetic Factors
Some cases of male infertility are tied to genetic conditions, such as Y-chromosome microdeletions or cystic fibrosis gene mutations. Genetic screening can help determine if such factors are at play.
How Male Fertility is Assessed for IVF
Before starting IVF, the male partner undergoes a comprehensive evaluation to assess his fertility potential. This usually includes:
- Semen Analysis: A detailed examination of sperm count, motility, and morphology.
- Hormone Testing: To check testosterone and other key hormone levels.
- DNA Fragmentation Testing: Assessing sperm DNA integrity, which can impact embryo quality.
- Physical Examination: Identifying any structural issues like varicocele.
- Genetic Screening: For men with unexplained infertility or a family history of genetic disorders.
Understanding male fertility through these tests helps fertility specialists choose the best course of action for the IVF process.
The Impact of Male Fertility on IVF Success Rates
While IVF can bypass certain male fertility issues, the quality of sperm remains pivotal to success. Poor sperm quality or DNA fragmentation may result in:
- Lower Fertilization Rates: Even with assisted methods like ICSI, sperm health affects the ability to fertilize eggs.
- Reduced Embryo Quality: Sperm issues can lead to embryos that fail to develop properly.
- Higher Risk of Miscarriage: DNA damage in sperm has been linked to early pregnancy loss.
In contrast, improving male fertility through targeted treatments or lifestyle changes can significantly enhance IVF outcomes. For example, men can improve their fertility by maintaining a healthy diet, exercising regularly, reducing stress, and avoiding harmful habits like smoking or alcohol abuse.
Treating Male Fertility Issues for IVF
If male fertility problems are detected, there are multiple ways to address them before or during the IVF process:
- Medical Treatments: Hormone therapy, surgery for varicocele, or antibiotics for infections.
- ICSI (Intracytoplasmic Sperm Injection): Directly injecting healthy sperm into the egg to bypass motility or morphology issues.
- Sperm Retrieval Techniques: For men with no sperm in their ejaculate, methods like TESA or Micro-TESE can retrieve sperm directly from the testes.
- Lifestyle Adjustments: Improving diet, exercise, and reducing exposure to toxins.
- Supplements: Antioxidants like Vitamin C, Vitamin E, zinc, and folic acid can help improve sperm health.
The Emotional Impact of Male Fertility in IVF
Fertility struggles are emotionally taxing for couples, and the role of male fertility is sometimes overlooked. Men often feel a mix of emotions—shame, guilt, or helplessness—when they learn their fertility is a contributing factor to infertility.
It’s important to emphasize that male fertility issues are common and treatable. Open conversations, emotional support, and counseling can help men cope with these challenges and remain actively involved in the IVF process.

Why Male Fertility Awareness is Crucial?
Despite being a crucial factor, male fertility often takes a back seat in discussions about assisted reproduction. Many men assume fertility is solely a female concern or feel hesitant to seek help due to societal stigma. This misconception can delay diagnosis and treatment, further reducing IVF success rates.
Raising awareness about male fertility helps normalize conversations around male reproductive health and encourages men to undergo timely evaluations. Proactive steps toward improving sperm health can make a world of difference for couples undergoing IVF.
Final Thoughts
Male fertility is an essential piece of the IVF puzzle. From sperm quality and quantity to lifestyle habits and genetics, numerous factors influence male reproductive health. By recognizing the role of male fertility and addressing any issues early, couples can maximize their chances of IVF success.
If you or your partner are considering IVF, remember that fertility is a shared journey. Male fertility matters just as much as female fertility, and prioritizing both can lead to a smoother and more hopeful path to parenthood. Whether it’s through lifestyle improvements, medical treatments, or advanced techniques like ICSI, solutions are available to address male fertility concerns.
Let’s break the silence around male reproductive health and ensure that everyone has the tools and knowledge they need to build their families. After all, fertility is not just a women’s issue—it’s a shared responsibility.


